November 7, 2014
Repeat Medical Imaging: A Classification System for Meaningful Policy Analysis and Research
HPI researchers propose a classification scheme that organizes repeat medical imaging into cohesive, clinically relevant categories for the research and clinical communities.
Introduction
As health care spending rises faster than the gross domestic product (GDP), considerable attention is focused on whether this growth is sustainable and whether it can be slowed without adversely impacting individual patient care or overall societal health. A consensus report dated September 6, 2012, released by the Institute of Medicine (IOM), indicates that an estimated $210 billion is spent annually on unnecessary medical services, while an additional $130 billion is wasted due to uncoordinated care.1 The Medicare Payment Advisory Commission (MedPAC) recently pointed to repeat testing as an area to explore for cost and waste reduction.2 More recently, Welch, et al. (2012) reported that repeat testing is common among Medicare beneficiaries; however, the authors failed to examine underlying medical necessity.3 Furthermore, the IOM has suggested the potential for substantial savings, estimating that $8 billion is spent annually on repeat testing. Although there is wide variation in reporting how much waste exists in our current health care delivery system and how it should be defined, there is consensus among researchers and policy makers that such waste exists and that action can be taken to reduce it. It is, however, the wide variation surrounding extremely large dollar amounts connected to patient care that makes taking action seem paradoxically attractive and risky.
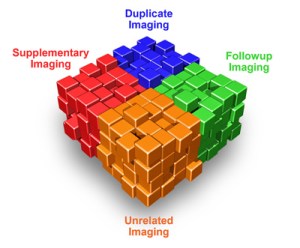
From both research and policy perspectives the term “repeat testing” is ambiguous and is often used to describe many different facets of both appropriate and potentially inappropriate care. For example, the universe of imaging studies that comprise “repeat imaging” could be conceived as the multi-faceted cube in Figure 1. While all of the imaging studies depicted would be appropriately classified as “repeat imaging,” each distinct facet represents a very different scenario of care. Even if a specific facet of health care is reviewed, such as mammography screening, data from unrelated clinical studies cannot be synthesized to provide a simple actionable plan to reduce cost. For an empirical perspective, a Google Scholar search on the terms “+ repeat testing + imaging” identifies 1,920 scientific papers since 2007. These papers span topics as diverse as examining patient adherence to mammography follow-up imaging guidelines and broad studies of the occurrence of multiple same-day imaging studies.
Because researchers typically study repeat testing within a specific clinical context, a rigorous classification system is warranted. Studies and policy remedies that seek to examine repeat testing for potential efficiencies may produce unintended consequences for overall quality of care if researchers and policy makers do not carefully consider the clinical context of a particular test—a problem that is only confounded by ongoing use of ambiguous terminology.
Although a repeat test is said to include elements already evaluated in a previous test for the same patient, most discussions have not adequately addressed the specific clinical circumstances under which such repeat testing may occur. Additionally, there is considerable lack of uniformity in defining the time frame in which subsequent testing is considered repeat testing or which tests might be construed as repeat tests with respect to an index examination.
With this background in mind, researchers at the HPI propose a classification scheme that organizes repeat medical imaging into cohesive, clinically relevant categories for the research and clinical communities studying this subject. Although our classification focuses on medical imaging, other health service providers and suppliers under the scrutiny of generic repeat testing analyses may find this framework useful in facilitating more meaningful analysis within their domains.
For any classification system of repeat services to be useful, it must be test specific so that it accounts for test characteristics that determine the appropriate time interval between tests and the clinical rationale that is the basis for these services. In the absence of such considerations, analyses may be too generic, and thus meaningless from a policy perspective because of misinterpretation or misapplication of data. The use of such non-specific analyses as the basis for policy making could result in immediate and unintended consequences for individual patients, as well as more permanent negative effects on the health care delivery system.
Proposed Classification System
Definitions:
Repeat testing: A diagnostic test that occurs within a test- or condition-specific time interval. Depending upon the clinical circumstances in which the subsequent test is performed, this could range from being entirely duplicative (or otherwise medically unnecessary) to complementary (such as to confirm, clarify, or stage a known or suspected process).
Repeat imaging: Medical imaging of the same anatomic site within a test- or condition-specific time interval.
The classification system proposed (Figure 2) pertains to imaging at the same anatomic site. Imaging of a distinctly different body part is, by definition, not repeat imaging, and should be studied separately.
For medical imaging, repeat testing is divided into four general categories: I) supplementary imaging, II) duplicative imaging, III) follow-up imaging, and IV) unrelated imaging. These are additionally subcategorized when appropriate to more robustly describe the clinical context in which such imaging may occur. Specific groups have been classified by color to indicate whether such imaging is typically appropriate and necessary (purple), typically represents an opportunity for improvement (yellow), or whether categorization alone provides insufficient evidence to so classify (light blue).
 |
| click image to enlarge |
I. Supplementary Imaging
Repeat medical imaging during the same or an overlapping clinical encounter involving a different imaging modality.
| a) High Value Added — A subsequent examination which either confirms or refutes the presence of a questionable finding identified on another examination or better characterizes a known abnormality or indeterminate finding. | |
|
A patient undergoes a non-contrast abdominal CT scan for evaluation of suspected kidney stones. A rounded low-density structure is identified in the left kidney that could reflect either a benign simple cyst or necrotic mass. A renal ultrasound (US) is then performed to distinguish. |
|
Since such studies are typically medically necessary, no clinical, behavioral, or structural changes would be anticipated to reduce their frequency. In fact, attempts to reduce utilization may actually impede high-quality patient care. |
| b) Low Value Added — One or more overlapping tests ordered during the same episode of care, of which one or more alone might be expected to answer the clinical question at hand. | |
|
A CT, US, and MRI of abdomen are all ordered at the same time for an inpatient with abdominal pain in the hopes that at least one of the studies will yield pertinent actionable findings. |
|
The results of the expected highest yield examination (using ACR Appropriateness Criteria® or other guidelines) would be the most likely to provide a definitive diagnosis, and thus may obviate the need for repeat imaging of the same body part during the same episode of care. This form of unnecessary use could be reduced with physician education and/or by the introduction of decision support at the point of order entry along with processes to more efficiently and effectively convey radiologist interpretations. |
II. Duplicative Imaging
Repeat medical imaging during the same or an overlapping clinical encounter involving the same imaging modality.
| a) Intentional Duplication — Repeat imaging is performed when providers are aware of previous similar examinations. In such circumstances, initial images and their interpretations may or may not be available, but patient or health system needs drive the repeat examination. | |
|
A CT done at hospital A at 11pm and repeated at hospital B at 3am the next morning, because neither images nor interpretation from the initial institution were available or accessible. The patient’s condition is such that the delay in obtaining the original images (or the interpretation thereof) would potentially result in suboptimal care.A patient with an unchanged headache returns to the emergency department four hours after discharge demanding a follow-up CT scan; her physician orders a repeat examination to assuage her.A patient with acute abdominal pain undergoes an abdominal CT scan overnight during admission. The next afternoon, his clinical condition deteriorates, and a subsequent CT examination is performed demonstrating interval bowel perforation. |
|
Unavailability of prior images and/or records, incorrect initial examination ordered and/or performed, patient demands, defensive medicine, suboptimal quality of original examination, different imaging protocol needed, or patient status change requiring new diagnostic information. |
|
When a patient’s clinical condition has changed and warrants further diagnostic evaluation, attempts to reduce the frequency of repeat imaging could prove harmful. Efforts to reduce intentional duplication should be directed at the root cause of follow-up imaging rather than at follow-up imaging in general. Intentionally duplicative imaging could be greatly reduced with improved integration of electronic health records (EHR) and medical imaging. Related improvements in health information technology (e.g., clinical decision support) can minimize incorrect initial testing. When patient expectations alone, rather than a compelling clinical need, drive repeat imaging, patient education could be helpful. Substantive and durable tort reform will be necessary, however, to fully resolve this driver of repeat imaging. If the quality of the original examination necessitated repeat imaging, efforts to systematically improve examination quality (unless patient factors were responsible in an individual instance) would be appropriate. |
| b) Unintentional Duplication — In this circumstance, the provider may not be aware that a previous, relevant examination exists. Accordingly, such a study is requested and performed as if it were a de novo examination. | |
|
A confused patient with chronic dementia presents to the emergency department at hospital A on Saturday morning. The clinical team does not know that the patient just underwent a brain CT at hospital B late Friday night. Another brain CT examination is ordered and performed. |
|
Unintentional duplicative imaging could likewise be greatly reduced with improved integration of electronic health records and improved portability of images. |
III. Follow-up Imaging
Repeat medical imaging during a subsequent related clinical encounter involving the same or a different imaging modality.
| a) Recommended Screening — A common form of repeat imaging takes place at scheduled time intervals to screen for cancer or other diseases. | |
|
An asymptomatic woman presents for an annual screening mammogram. |
|
Since these studies are typically medically necessary, no clinical, behavioral, or structural changes would be anticipated to reduce their frequency. In fact, attempts to reduce utilization may actually impede high-quality patient care. |
| b) Standard Follow Up or Surveillance — Repeat imaging is performed at intervals dictated by clinical circumstances or accepted guidelines to evaluate progression, regression, or recurrence of a known disease. | |
|
Patients with actively treated or previously treated cancer are imaged to tailor chemotherapy or survey for recurrent disease, respectively. |
|
Since these studies are typically medically necessary, no clinical, behavioral, or structural changes would be anticipated to reduce their frequency. In fact, attempts to reduce utilization may actually impede patient care. |
| c) Non-Standard Follow Up or Surveillance — Unwarranted additional imaging such as that related to the ordering of examinations more frequently than recommended at the time of an initial interpretation, or related to radiologists’ non-conformance with established guidelines in report recommendations. | |
|
A chest CT examination performed for other reasons demonstrates an incidental 5-mm solitary lung nodule in a non-smoker. The radiologist recommends a follow-up examination at three months when published guidelines indicate a repeat examination at 12 months would suffice. |
|
Existing evidence-based guidelines should guide practitioners to recommend and request examinations at intervals outlined in consensus documents. Incorporating real-time decision support into ordering and reporting systems could improve conformance. |
| d) Inaccessible Prior Imaging Information — Follow-up imaging might be obviated if a complete historical imaging record were accessible, (e.g., ambulatory patients who change residence but don’t retain previous medical records, leaving a physician in the new location with limited or no historical information). | |
|
A patient has an indeterminate adrenal nodule previously identified and subsequently established as stable and benign. In the absence of an accessible, transferable medical record, a CT examination at a later date in the new location demonstrates a “new” nodule, necessitating another round of radiologic work up to establish benignity. |
|
Electronic health record integration and health information exchanges may help minimize such occurrences and improve overall patient care. |
IV. Unrelated Imaging
Repeat medical imaging during a subsequent unrelated clinical encounter involving the same or a different imaging modality.
| a) Unrelated Event — A patient encounter that occurs for an entirely different purpose. | |
|
A patient undergoes CT of the abdomen and pelvis for breast cancer staging two weeks prior to a motor vehicle collision; another CT of the abdomen and pelvis in the acute setting is required given her clinical presentation and the mechanism of injury. |
|
Since these are typically medically necessary tests, no clinical, behavioral, or structural changes would be anticipated to reduce their frequency. In fact, attempts to reduce utilization may actually impede patient care. |
 |
Recommendations
The term “repeat testing” as currently used is neither precisely nor universally defined. When investigating the appropriateness of a repeat test, investigators must precisely define their methodology, specifically as it pertains to the clinical context in which such services are performed. Without precision and uniformity, further investigation may result in health care policy which could unintentionally impede the quality of individual patient care and overall societal health.
Additionally, investigators should use the correct data for targeted analyses of repeat testing and perform their studies in meaningful clinical contexts. In some cases, administrative data may be sufficient, particularly when used by physicians with clinical expertise in a specific domain. However, in many cases actual clinical data will be required for rigorous analysis. Integrated electronic records data may be one way to identify clinical nuances, particularly when they apply to unintentional duplication.
The researchers at the Harvey L. Neiman Health Policy Institute propose this classification system to facilitate more meaningful analyses and serve as the basis of improved adherence to and development of evidence-based guidelines and health information technology that advance patient care and simultaneously reduce duplication and waste.
Resources
- Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Available at: https://www.nap.edu/catalog/13444/best-care-at-lower-cost-the-path-to-continuously-learning. Accessed September 6, 2012.
- Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System, June 2012. Available at:http://www.medpac.gov/docs/default-source/reports/march-2012-report-to-the-congress-medicare-payment-policy.pdf?sfvrsn=0. Accessed September 7, 2012.
- Welch HG, Hayes KJ, Frost C. “Repeat Testing Among Medicare Beneficiaries.” Arch Intern Med. 2012;172(22):1745–1751.