December 16, 2015
Neiman Imaging Types of Service (NITOS)
Neiman Imaging Types of Services (NITOS) codes provide a variable that can be merged into datasets by HCPCS code to identify imaging procedures by modality and anatomic site. This new coding system augments the existing BETOS system for imaging focused studies, and was designed to be usable either in conjunction with or in lieu of BETOS for imaging analyses.

A New Classification System for Non-Invasive Diagnostic Imaging Professional Services Using Payer Claims
Introduction/Rationale
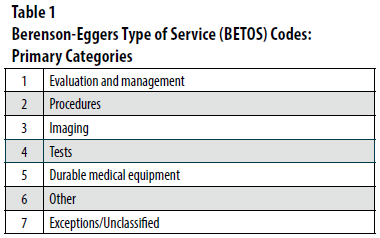
The Center for Medicare & Medicaid Services (CMS) developed the Berenson Eggers Type of Service (BETOS) coding system primarily to facilitate analyzes of ongoing growth in Medicare expenditures1. BETOS assigns each billing Healthcare Common Procedure Coding System (HCPCS) code to one of seven broad BETOS categories (Table 1). These categories include imaging, and are further subdivided into a larger number of subcategories. The groupings are intended to be objective, readily understood, and clinical (rather than statistical or financial) in nature. In addition, the categories were designed to remain largely stable, avoiding marginal changes over time in technology or clinical practice.
To date, the BETOS coding system has served CMS and the health policy and health services research community well, providing a common lexicon for identifying types of medical services. BETOS has been instrumental in helping policy makers and health services researchers identify trends and changes so as to guide a variety of payment distribution and utilization management efforts.
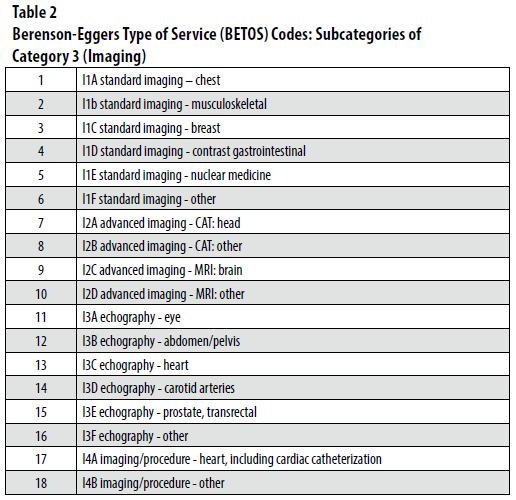
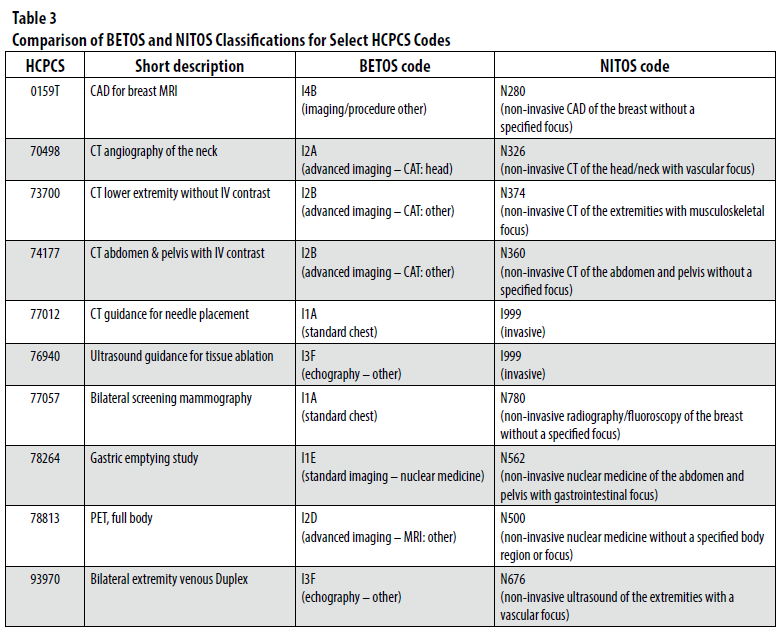
Despite its many favorable attributes, the BETOS coding system is not without problems, particularly as it relates to identifying further subcategories of services within individual specialty areas. Medical imaging—the focus of considerable policy attention in recent years—is one such area. Imaging services are classified by BETOS with the letter “I” and further grouped into 18 subcategories (Table 2), loosely based upon modality. Specifically, imaging codes are first subcategorized as “standard imaging” (referring to radiography and nuclear medicine), “advanced imaging” (referring to CT and MRI), “echography” (an outdated term referring to ultrasound), or as “imaging/procedure” (largely a generic “everything else” grouping). Further subclassification by BETOS, however, lacks meaningful clinical granularity. For example, CT and MRI are each divided into “head” (CT) or “brain” (MRI) vs. all other CT/MRI exams—the latter obviously representing a huge number of highly varied services. In addition, a number of inaccuracies exist within the classification system. For instance, while a subcategory exists for imaging of the breast, certain types of mammography (e.g., HCPCS code 77057 for bilateral screening mammography) are instead categorized incorrectly as chest imaging. Similarly, some codes for positron emission tomography (PET) imaging—specialized types of nuclear medicine examinations—are classified as either ultrasound or MR, which are both incorrect. Moreover, despite the presence of dedicated procedural categories within BETOS, a number of procedural codes are included in the standard imaging and echography categories [e.g., HCPCS code 77012 for CT guidance for needle placement for any of a number of procedures performed anywhere in the body is categorized as standard (not CT) imaging of the chest]. Such categorization errors greatly limit the applicability of BETOS for targeted analyses relating to interventional radiologists. These observations (just examples of many others) raise concerns regarding the appropriateness of BETOS for sophisticated granular-level analyses of trends related to medical imaging. Given considerable recent attention to imaging utilization, with regards to both radiation dose to the population as well as its cost, the limitations of BETOS will likely continue to hamper its use in claims-based studies.
As medical imaging becomes increasingly subspecialized, a robust classification system is necessary to help better support health services researchers and policy makers in their efforts. The array of imaging professional services rendered by radiologists continues to grow in nuanced complexity with progressive advances in technology and clinical practice. This evolution further challenges the ability of BETOS to optimally capture emerging practice patterns. For example, neuroradiologists interpret imaging of the brain, but commonly of the spine and head and neck as well. Only brain imaging, however, is uniquely identifiable in BETOS. Additionally, as previously noted, standard imaging categories in BETOS include a number of codes that more appropriately belong in other groups.
In order to address such issues and needs, and to provide a platform for ongoing meaningful claims-based imaging health services research focusing on non-invasive diagnostic imaging professional services, we have developed the Neiman Imaging Types of Services (NITOS) coding system. This new coding system augments the existing BETOS system for imaging-focused initiatives, and was designed to be usable either in conjunction with or in lieu of BETOS for imaging analyses. This policy brief describes the key elements of the NITOS coding system.
Methods
Publicly available Medicare Provider Utilization and Payment Data files were obtained from CMS2. These files contain information for 100% of Part B non-institutional services and procedures rendered to Medicare fee-for-service beneficiaries by physicians in 2012 and 2013. All HCPCS codes for which claims were filed during those two years by a physician listed in the CMS database as a radiologist were identified. We defined a radiologist as a physician self-designating to Medicare using a specialty of either diagnostic radiology, nuclear medicine, or interventional radiology. Of these, all codes classified as imaging by BETOS (i.e., assigned a BETOS category of “I”) were selected for further assignment of a NITOS category. Short descriptors of the HCPCS codes were obtained from the Medicare Physician Fee Schedule3, and the 2015 edition of the Current Procedural Terminology (CPT) Professional Edition code set4 was consulted for more detailed descriptions of codes as needed. Codes identified as imaging by BETOS not referring to professional services (e.g., pharmaceuticals or other supplier codes) were excluded from further classification given the current intent of NITOS to inform research relating to radiologists’ actual work patterns (e.g., subspecializaton trends).
Two radiologists with experience in Medicare claims-based health services research reviewed and classified all radiologist-billed HCPCS codes using the NITOS coding scheme introduced in this policy brief. Both are board certified in diagnostic radiology; one is fellowship trained in abdominal imaging and the other in interventional radiology. One has served on the CPT Editorial Panel (the organization which maintains the CPT code set) and its executive committee. The radiologists initially assigned code categories independently, and then discussed areas of discrepancy until reaching agreement for all codes.
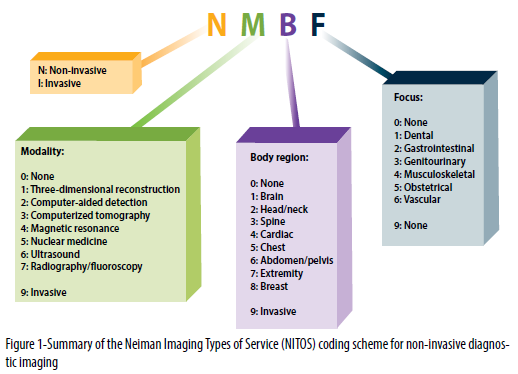
NITOS applies a hierarchical structure for coding diagnostic imaging professional services, as outlined below and in Figure 1:
- Codes related to professional services rendered by radiologists are initially classified as either invasive (I) or non-invasive (N). Invasive codes include percutaneous diagnostic imaging procedures as well as therapeutic imaging procedures of any nature. Currently, invasive codes are not further subclassified.
- Non-invasive diagnostic imaging professional service codes are further classified by both modality (3D reconstruction, computer-aided detection, computed tomography, magnetic resonance, nuclear medicine, ultrasound, or radiography/fluoroscopy) and body region (brain, head/neck, spine, cardiac, chest, abdomen/pelvis, extremity, or breast). A body region of “none” was assigned for imaging examinations that routinely image numerous body regions or the entire body (e.g., HCPCS 78306 for nuclear medicine whole-body bone scan and HCPCS 77075 for radiographic complete skeletal survey), as well as for targeted exams that could be applied to any of a number of individual body regions (e.g., HCPCS 78811 for PET of a limited area).
- Non-invasive codes were also assigned an additional “focus” when a specific organ system focus could be confidently stated for the given examination. This applied to only a minority of services. Specific focus areas identified were: dental, gastrointestinal, genitourinary, musculoskeletal, obstetrical, and vascular. When no single unique focus was confidently identifiable (e.g., an abdominal CT examination could focus on gastrointestinal and/or genitourinary pathology), none was assigned.
To summarize, NITOS classifies each HCPCS code for imaging professional services billed to Medicare by radiologists in 2012 and 2013 as invasive or non-invasive. When non-invasive, NITOS subclassifies the code by both modality and body region. When applicable, an additional focus area is assigned. Single-digit numerals are used to designate each modality, body region, and focus area (Figure 1), with these three parameters being assigned a “9” for invasive codes. Table 3 provides a comparison of BETOS and NITOS classifications for selected HCPCS codes.
Discussion
In this brief, we have outlined the initial development of NITOS, a new scheme intended to provide a comprehensive and reliable classification of HCPCS codes for non-invasive diagnostic imaging professional services. This new coding classification system addresses gaps and inaccuracies in the current BETOS scheme as they pertain to imaging. The aim of NITOS is not to replace BETOS for health services and health policy research related to imaging, but rather complement it depending on the context of particular investigations. For higher-level analyses evaluating general trends in the use of imaging, BETOS is likely to continue to be used given its broad acceptance within the health services research community and ability to reasonably and reliably identify imaging services as distinct from other healthcare services. On the other hand, for targeted analyses requiring a more granular classification of specific non-invasive diagnostic radiology professional services (e.g., studies of diffusion of technology amongst subcategories of imaging examinations or investigations relating to subspecialty radiologists’ work patterns), NITOS will likely prove more useful.
We intend to maintain full transparency regarding the NITOS scheme. Accordingly, the full classification system will be maintained in a publicly available manner on the Neiman Health Policy Institute website5. Updates, revisions, and corrections will be posted as they become available (e.g., next CMS release of provider claims summary data) or necessary. With regard to the latter, its developers welcome commentary from the radiology and health services and health policy research communities. We encourage interested stakeholders to review the classification scheme and provide feedback regarding the system. Our goal is that NITOS will prove itself to be a valuable tool for improved insights for policy-focused claims-based research relating to non-diagnostic medical imaging professional services.
References
- Center for Medicare & Medicaid Services website. Berenson-Eggers type of service (BETOS). http://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/BETOS.html. Last modified November 12, 2014. Accessed August 13, 2015.
- Center for Medicare & Medicaid Services website. Medicare Provider Utilization and Payment Data: Physician and Other Supplier. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier.html. Last modified June 1, 2015. Accessed August 13, 2015.
- Center for Medicare & Medicaid Services website. Physician Fee Schedule. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/index.html?redirect=/PhysicianFeeSched/. Last modified May 11, 2015. Accessed August 15, 2015.
- American Medical Association. CPT 2015 Professional Edition. Published 2014.
- Harvey L. Neiman Health Policy Institute. http://www.neimanhpi.org/. Accessed on: August 13, 2015.
Authors
Andrew Rosenkrantz MD MPA,
Affiliate Research Fellow, Neiman Institute
Associate Professor, NYU School
of Medicine